SKIN DISORDERS
Persons with skin disorders must also clean and care for their skin
Effective treatment encompasses:
- stabilizing the acid mantle
- stabilizing other protective mechanisms
- and through these measures, increasing the skin’s resilience
The following skin diseases are discussed:
- Acne and skin impurities (oily)
- Allergic reactions (sensitive)
- Contact dermatitis (sensitive)
- Atopic dermatitis/eczema (dry)
- Psoriasis (dry)
- Viral, bacterial and fungal infections
- Rosacea
- Seborrhoeic eczema
ACNE AND SKIN IMPURITIES
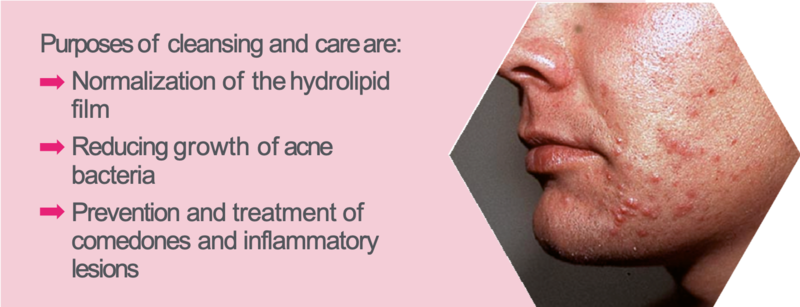
- Skin is oily
- Usually occurs with the onset of puberty, caused by changes in hormones
- Clinical manifestation defined by comedones, pustules, papules and fistula
Purposes of cleansing and care are:
- Normalization of the hydrolipid film
- Reducing growth of acne bacteria
- Prevention and treatment of comedones and inflammatory lesions
Acne (acne vulgaris) is the most common dermatological disease. It affects young people in particular, of whom about 80 % have lesions on the face, chest and back. The pathogenesis involves an increased production of hormones (androgens).
Male adolescents are affected more often and more strongly than females. The disease peaks at between 15 and 20 years of age. After puberty, in most cases a spontaneous regression occurs. Depending on the severity and duration of the disease medical treatment may be required. Acne can also persist or, more rarely, only occur in later years (acne tarda).
The clinical symptoms are open (blackheads) and closed (whiteheads) comedones, papules, nodules, pustules and sometimes abscesses and fistulas. The skin is usually oily with enlarged pores. Different degrees of severity are distinguished depending on the kind of lesions:
- Acne comedonica (mild form with few comedones, papules and pustules)
- Acne papulo-pustulosa (moderately severe form with papules, pustules and nodules)
- Acne conglobata (a severe type with cysts, fistulas and nodules)
The pathogenesis of acne consists of seborrhea combined with hyperkeratosis of the ducts of the sebum glands, increasing bacterial colonization (Propionibacterium acnes) and additional factors such as use of comedogenic substances, stress, diet or UV radiation.
The underlying skin condition is oily. In addition to the therapeutic measures with keratolytic and antibacterial agents, the normalization of the sebum is the most important approach to care. For cleansing, a soap-free cleansing bar or a mild cleansing foam at pH 5.5 and a clarifying toner that removes excess sebum and soothes the skin is recommend. It is important to care for the skin adequately. Oil-free gels, oil- and emulgator free hydridisperion gels or water-in-oil emulsions with low oil content are recommended.
ALLERGIC REACTIONS

Therapeutic measures:
Purposes of cleansing and care are:
The skin functions as an immune organ through Langerhans cells in the epidermis and the dermis and with the help of mast cells, leukocytes and lymphocytes. Triggering stimuli do not only pass through the skin but may also be caused systemically, e.g. as a result of food allergy.
Allergic reactions occur only after a previous contact with a sensitization to the allergen. The initial contact induces no visible skin reaction but an immune response. Antibodies making the allergic reaction possible and an immunologic memory imprint must be created. After this sensitisation process any further contact with the allergen induces an immune response leading to the development of the typical symptoms of an allergy.
Ig-E mediated reactions are known as immediate type hypersensitivity reactions (type 1). Here, the antibodies are not found in the lymphocytes after sensitization but are located in the mast cells of the skin.
An allergic reaction usually manifests by the appearance of blemishes and redness that can affect large areas of skin as well as wheals or edema.
The first therapeutic measure is the administration of antihistamines and strict avoidance of the allergenic trigger (if known).
As the skin is irritated, it is important to reinforce the skin’s barrier further so no additional damage can occur. In order to stabilize the acid mantle and the barrier function, a mild soap-free cleansing product should be used.
Skin care products should not be used on affected skin until the symptoms of inflammation have disappeared. For the surrounding skin and the site of reaction after fading of the inflammation, care products used should have a pH of 5.5 and contain skin calming substances. Phytosterols from rapeseed oil are suitable. Topical application of preparation with highly concentrated Phytosterols has an anti-inflammatory effect.
- As an immune organ, the skin can be affected by immediate type allergic reactions
- Urticaria (hives) with appearance of spots, reddening or wheals at the point of contact and edema are possible
- Antihistamines
- Avoiding contact with the source (abstention)
- Strengthening the skin’s barrier
- Alleviating redness and itching
CONTACT DERMATITIS

- Allergic reactions or irritated skin after topical contact with substances such as nickel or the ingredients of low quality skin care products
- Symptoms include reddening, stinging, itching, nodules, blisters or swelling at the site of contact
Purposes of cleansing and care are:
- Stabilizing the immune system by
- re-establishing the skin’s protective mechanisms
Dermatitis (or eczeme) is a non-infectious skin disease which manifests in skin inflammation. Contact dermatitis is a skin reaction to certain substances applied locally.
We can distinguish:
Allergic contact dermatitis
Toxic-irritative contact dermatitis
The risk for developing an eczema is enhanced by a disturbed barrier layer and bacterial or fungal infections. Eczematous skin is extremely sensitive.
In case of a contact allergy any contact with the allergen is problematic because the substance causes a release of antibodies. As a result, an inflammatory response is triggered. This can be identified by redness, papules and vesicles. The skin weeps and itches. Normally, the reaction is limited to the contact site of the allergen.
Allergic contact dermatitis is a delayed-time immune reaction (type IV) which means that the onset of the reaction occurs within 24 hours and the culmination of the reaction within 48 hours. This type of reaction is mediated by
T-lymphocytes and requires asymptomatic sensitization prior to the reaction just as immediate type reactions do.
Typical contact allergens are: nickel, both as jewelry and as production residues in cosmetics of poor quality and purity, certain preservatives, perfumes and lanolin. The most important therapeutic measure is the avoidance of the allergen.
Toxic irritative contact dermatitis is a non-immunological inflammation. The reaction occurs shortly after initial contact. No sensitization is required.
A special form of skin reaction is termed “stinging“. This is a burning sensation without irritation or inflammation which usually subsides 10 to 20 minutes after contact.
In cleansing and care, stabilizing the skin barrier of sensitive individuals is important. Consequently cleansing must be soap-free at pH 5.5 to support the protective acid mantle.
ATOPIC DERMATITIS
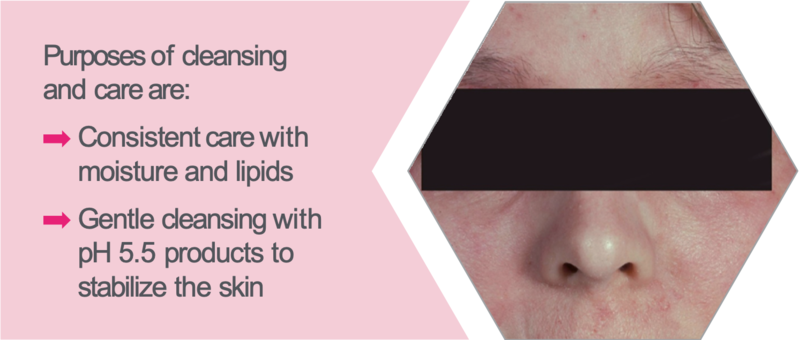
- Chronic or chronically relapsing, noncontagious skin disease usually associated with severe itching
- Age dependent with differing forms and locations
- Skin is dry
Purposes of cleansing and care are:
- Consistent care with moisture and lipids
- Gentle cleansing with pH 5.5 products to stabilize the skin
Atopic eczema or atopic dermatitis is a chronic, non-infectious, recurring skin disease associated with dry skin and intense itching. There is a genetic disposition to develop hypersensitivities of the skin as well as the respiratory tract.
A decreased skin barrier function and increased responsiveness of the immune system render the skin susceptible for severe and long-lasting inflammation. Triggers can be infections, hormones, mental stress or environmental factors such as the climate, environmental allergens, food or irritating substances. In addition, the defense of the skin against bacterial, fungal and viral pathogens is impaired. This sometimes leads to secondary infections in the inflamed areas of skin. In some patients there is a general colonization of the skin with Staphylococcus aureus.
The appearance and localization is dependent on age. The disease frequently occurs already in infants. In acute cases, the skin is inflamed and weeps.
Known pathogenic factors are a disturbed water-binding capacity of the skin by a lack of moisturizing factors (e.g. urea), a defect in cohesion of the corneocytes due to defient filaggrin production and a lack of epidermal
lipids. This is likely an enzyme defect (delta-6-desaturase) leading to a disorder of the lipid metabolism and to a lack of anti-inflammatory prostaglandins.
The condition of the skin outside of the acute stage is dry.
In addition to therapeutic treatment with corticosteroids, topical calcineurin inhibitors, antipruritics, antiseptics and antihistamines, the consistent application of emollients and moisturizers is an established basic requirement for the reduction of flare-ups of eczema: Urea, for example. For the long-term treatment with lipids and moisturizers, phytosterols, in particular, are often used.
As the skin should not be irritated in any case, maintaining a pH of 5.5 is optimal. At this pH value the damaged acid mantle is stabilized and a superinfection with bacteria may be prevented.
PSORIASIS

- Chronic disease with accelerated cell division in the basal cell layer which leads to scaly skin thickening (plaques)
- Symptoms: dry, itchy skin
Purposes of cleansing and care are:
- Skin care with mild cleansing and personal care products for dry, sensitive skin in order to stabilize the skin’s barrier function
Psoriasis is a chronic disease of the skin, internal organs and joints. It is an autoimmune disease; the exact trigger is not yet known. The most common manifestation, psoriasis vulgaris, is shown on the skin, particularly the epidermis. The keratinization of epidermal cells is disrupted due to an increased rate of cell division in the basal cell layer. The cell renewal process is reduced to 3 to 4 days (instead of 28). The keratinocytes on the way to the surface do not complete their normal differentiation and cannot be desquamated leading to plaque formation. Dilated blood vessels cause redness in the afflicted areas and an increased level of leukocytes can also occur resulting in recurring inflammation. The skin is generally very dry.
Clinical manifestation presents as hyperkeratinized, scaly patches, usually silvery-white with erythematous areas that are clearly demarcated. Typical sites are the extensor surfaces of joints, the scalp, lower back and buttocks.
Psoriasis affects between 2 - 3 % of the population. The incidence varies depending on geographical location (Source: German Psoriasis Association). The disease may first appear between the ages of 15 to 20 years (type I) or from the age of 50 (Type II).
Several factors can trigger psoriasis activation, including physical stimuli such as scratching and abrasion or chemical stimuli such as solvents or soaps.
Depending on severity, medical treatment is effective with keratolytic, anti-inflammatory agents and Vitamin D analogues to inhibit proliferation or with immuno-suppressants.
In care, it is important that a mild soap-free cleanser adjusted to pH 5.5 is used to prevent further irritation. Care during the day is carried out with lipid-rich O/W emulsions and at night with W/O emulsions. The stabilization of the barrier function is the most important goal in skin care.
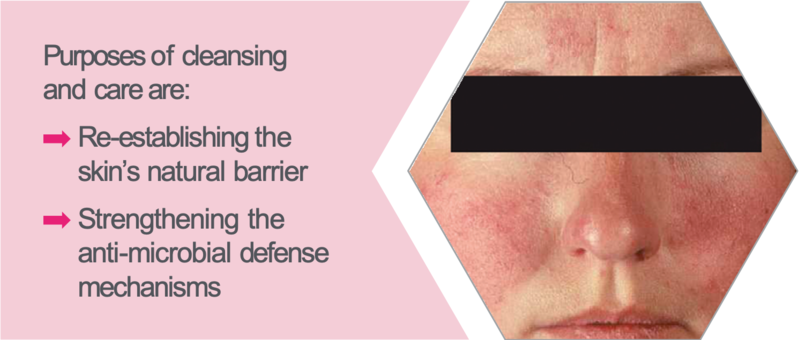
SKIN INFECTIONS
Viral, Bacterial and Fungal Infections

- Viruses bacteria or fungi in conjunction with a weak immune defense in the skin can lead to infections
- Symptoms: redness and inflammation
- Therapeutic measures: anti-inflammatory, anti-bacterial or anti-fungal medication
Purposes of cleansing and care are:
- Re-establishing the skin’s natural barrier
- Strengthening the anti-microbial defense mechanisms
Bacterial infections (Impetigo) occur in injured skin or skin with weak immune protection. This means that the protective acid mantle, which normally prevents the penetration of pathogenic bacteria is not intact.
Nonspecific bacterial infections are often due to staphylococci or streptococci. Clinical manifestation is not very specific.
Fungal infections (mycoses) are most likely to occur in areas that are moist, causing skin deliminated signs of inflammation.
Therapeutic measures consist of the local application of antibiotics, antiviral or antifungal agents. In severe cases with recurrent or prolonged symptoms, systemic therapy is required.
The most important care objective is to restore the natural skin barrier: the acid mantle and epidermal lipids. Cleansing and skin care products should be adjusted to pH 5.5 possibly with additional anti-inflammatory agents such as Allantoin and Bisabolol.
The pH value is of great importance as a part of infection prevention. At a pH of 5.5, as with sebamed products, the natural defense mechanism of the acid mantle is optimally supported. This provides a pH environment which favors the growth of non-pathogenic bacteria and keeps the growth of pathogens low. The products do not have disinfecting effect but influence the skin flora positively.
For the recommended general prophylactic practice of washing the hands, sebamed skin cleansing products also offer advantages: in addition to inhibiting the growth of pathogenic microorganisms through the acidic pH, they also support the skin’s barrier and protect against dryness and irritation.
ROSACEA
- Persistent facial redness on the nose, chin and cheeks: Couperosis
- Sensitive, easily irritated skin
- Rough, scaly skin
- Transition to Rosacea possible with symptoms, such as vasodilation with nodules and pimples on the nose, forehead, chin and areas of the cheek
Purposes of cleansing and care are:
- Re-establishing the skin’s natural barrier
- Strengthening the anti-microbial defense mechanisms
Constant, noticeable facial redness is known as couperose skin as the arterial vasodilation creates a bright red glow. Initially a temporary redness appears in the naso-labial folds and on the cheeks. With the increased incidence the redness persists due to blood remaining in the dilated capillaries. Sometimes this leads to a formation of new vessels which have a higher permeability and induce a permanent visible reddening of the face.
Sensitive, easily irritated skin is susceptible to this condition and usually associated with a connective tissue weakness. Women between the ages of 30 and 50 are affected more than men. Causes are often physical (e.g. prolonged exposure to cold) or chemical irritation through improper care but also through diseases such as hypertension or the onset of rosacea.
Rosacea is chronic and usually recurring. The course of the disease leads to permanent extensions of the superficial blood vessels in the skin and scale formation. Later pustules, nodules or swelling may occur.
The cause is not clearly understood. A genetic predisposition seems to play a role. Physical and chemical irritation often triggers the disease. In some cases it develops from a couperose skin.
A mild, soap-free cleanser with pH 5.5 is recommend to restore the acid mantle and increase the resilience of the skin. In skin care it is important that moisturizing products with pH 5.5 and a low oil content are used so that the skin is not further irritated.
Intense exposure to the sun should be avoided and if it can not be prevented, then care must be taken to provide consistent UV protection with a high SPF. In rosacea, all influencing factors (aside from the sun: cold, stress, alcohol, hot spices) should be avoided. Antibiotics (metronidazole) and antifungal agents can be used in therapy.
SEBORRHOEIC DERMATITIS
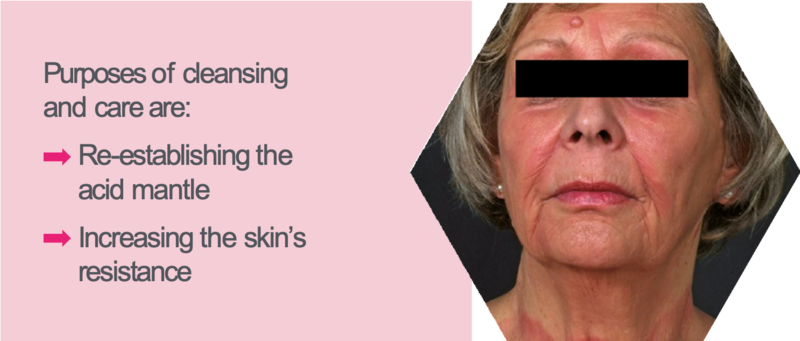
- Oily, scaly inflamed skin in areas that have many sebaceous glands
- Triggers are fungal infections of the hair follicles
- Affects infants and adults
Purposes of cleansing and care are:
- Re-establishing the acid mantle
- Increasing the skin’s resistance
Seborrhoeic dermatitis (seborrhoeic eczema) is an inflammatory disorder that typically manifests itself with scales and yellowish crusts. Itching, while present in some cases, is not marked. The disease‘s course is often long, sometimes even chronic.
Affected areas are where many sebaceous glands are present. Generally this is the head and face, eyelids, nasolabial folds or even the back and the chest. Men are affected more often than women.
Seborrhoeic dermatitis may also occur in infants where the head is afflicted. This particular form is known as cradle cap.
In adults, the sebum production is greatly increased and skin renewal is disturbed. Large yellowish, oily scales flake off and contrast to the fine whitish scales of dry skin.
The inflammation of hair follicles in the skin is caused by fungi (Malassezia furfur = Pityrosporum ovale and Pityrosporum orbiculare). Sebum is the source of nourishment for the skin fungi so that they multiply excessively. The degradation products of sebum act as irritants.
In addition to a genetic predisposition, influencing factors are hormones (testosterone), climate, moisture and physical irritation caused by improper care products. Therapeutic treatment is with antifungal and keratolytic agents.
For cleansing a mild, soap-free product adjusted to pH 5.5 is optimal. It is important not to irritate the skin and reinstate a pH of 5.5 so the fungal growth is curbed. The skin should then be lightly moisturized with a product containing soothing additives such as Allantoin.
