Our Skin …
- Is our largest organ
- Is functionally separated into multiple layers
- Protects the inner body like a coat of armor from harmful environmental influences
- Fulfills important tasks in the regulation of bodily functions
- Defines our appearance
- Is a habitat for billions of micro-organisms - helpful as well as harmful species
- … and needs individualized cleansing and care!
With a surface area of 1.5 to 2 m2, our skin is the largest human organ. Its weight is about 16 % of the total body weight.
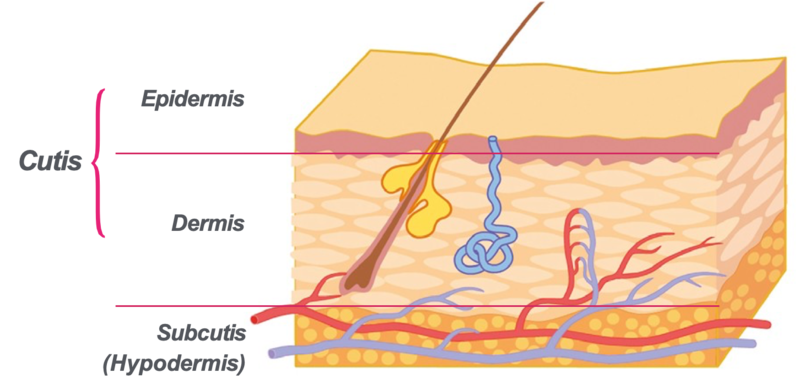
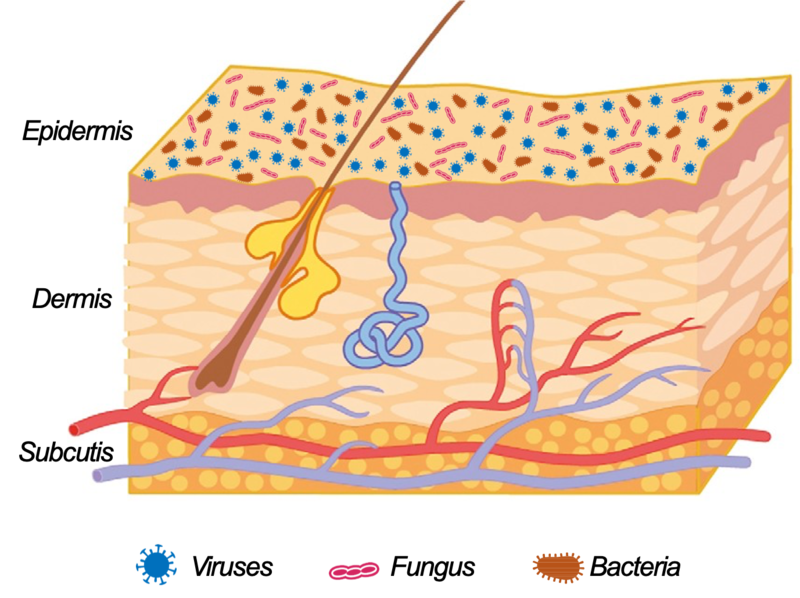
The skin is the outer boundary of our body, yet in most places it has a thickness of only several millimeters. The anatomy of the skin is structured into three layers: the epidermis, dermis and the subcutis.
In addition, the skin fulfills important tasks such as defensive and protective functions or sensory perception of touch, itch and pain as well as temperature control. Intact skin is an effective chemical, physical, microbiological and immunological barrier providing protection with the help of special, constantly renewing lipids and enzymes (structural and functional elements).
In addition to these defense functions the skin provides protection against dehydration. Due to this mechanism the skin controls its resistance and appearance while simultaneously controlling the temperature of the body.
The skin is also a complex ecosystem. Research in the composition of the skin microbiome has just started, indicating that there are complex interactions of ourselves and the various microorganisms present in and on the skin.
An intact structure and function in the skin is important because it is the only way it can fulfill its multiple functions and provide optimum protection. For this, individualized skin cleansing and skin care is necessary. This allows the skin to remain healthy or acts to supplement specific care ingredients for the treatment of problematic skin and skin deficiencies in order to regenerate the function of the skin.
THE SKIN’S STRUCTURE
To illustrate how complex the skin structure is, first a few facts and figures:
A square centimeter of skin contains an average of 3 million cells, 100 sweat glands, 15 sebaceous glands and, depending on the location, 50 - 200 pain receptors as well as about 1000 mm of blood vessels. 5 temperature receptors per square centimeter act as ‘sensors‘ for temperature in the palm of the hand while the face has 25 per square cm.
Our skin is clearly divided into three main layers:
- Epidermis
- Dermis
- Subcutis
The deepest layer of the skin, the subcutis, is separated from the interior of the body through a layer of connective tissue (fascia). This is composed of fat cells separated by loose connective tissue. The fatty tissue of the subcutis plays a role as a mechanical cushion and impact protection for the internal organs. It also provides protection from the cold and is the main energy reserve of the body. With increasing age there is a redistribution and in some cases a reduction of subcutaneous fat which influences the outward appearance of older persons.
The characteristics of the subcutis are also responsible for a cosmetic problem: cellulite (dermopanniculosis deformans). This is a an alteration in the topography of the skin’s surface which occurs particularly on the buttocks and thighs.
In the subcutis there are also sweat glands and parts of the hair follicle. Together with the sebaceous glands and nails they are skin appendages which are formed in the epidermis and anchored in the dermis or subcutis.
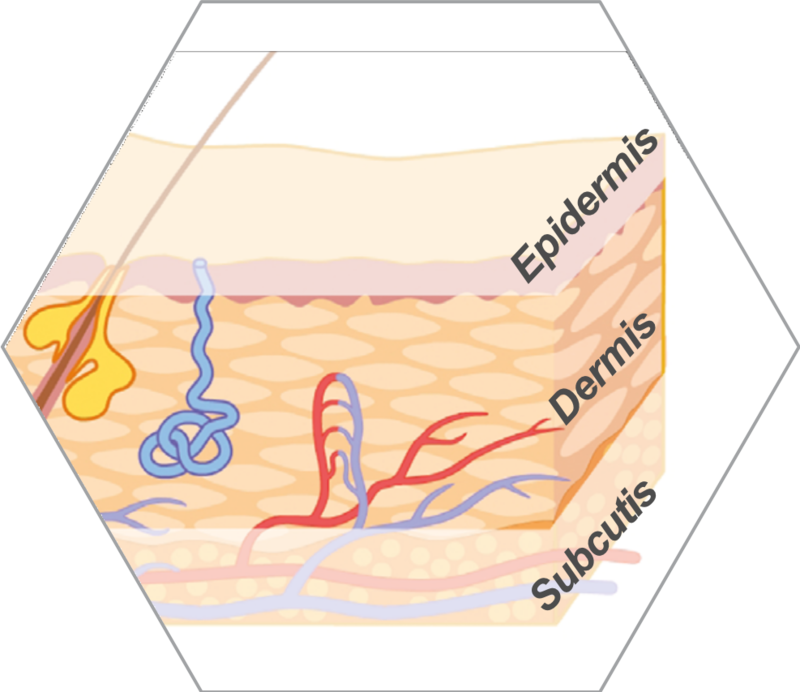
The Dermis
- Situated between the subcutis and epidermis
- Composed of perfused connective tissue with lymph and blood vessels and nerve fibers
- Structure defined by protein fibers in an extracellular matrix
- Dermal tissue cells produce collagen and elastin, matrix proteins and enzymes
- Fulfills multiple functions including as an immune barrier, providing skin sustenance and sensory perception
The dermis - also called the corium - is a very resilient, tear-resistant tissue which is located between the epidermis and subcutis. The tissue is composed mainly of connective tissue fibers (collagen and elastin) and cells that are embedded in a gel-like matrix. Collagen fibers are relatively rigid and are responsible for the mechanical stability and tensile strength of the skin. The elastic fibers are rubber-like and ensure that the skin can stretch and return to its original shape.
The matrix is gel-like and is composed of water binding glycosaminoglycans including the well known Hyaluronic acid. The function is the maintenance of water and electrolyte balance, tissue pressure and the viscoelasticity of the skin.
The most common dermal tissue cells are fibroblasts which produce glycosaminoglycans, collagen and elastin as well as matrix proteins and enzymes. In additon mast cells, lymphocytes, leucocytes and macrophages are located in the dermis which play an important role in the immune system.
The transition to the epidermis (outer layer) contains dermal papillae: small, nipple-like extensions of the dermis into the epidermis. In this area, the collagen fibers are finer and there are more vessels. Through this, the skin becomes more resistant to external forces and strain.
The dermis is structured into two layers: the papillary dermis (upper section) and the reticular dermis (lower section). The dermis also contains nerves and the basis of skin appendages with their supporting blood and lymph vessels.
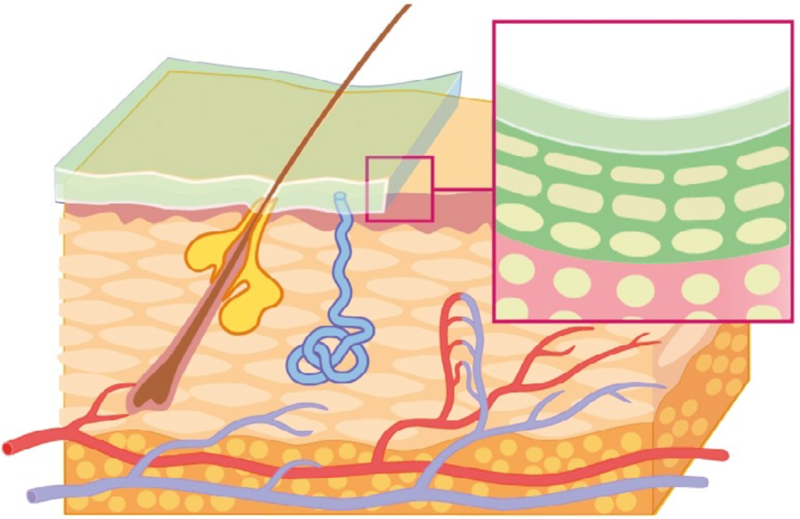
The Epidermis
- Outer layer, subdivided into three strata, which gives the human skin its typical appearance
- Together with the Stratum corneum (horny layer) the epidermis forms the outer protective boundary of our body
- Squamous epithelium composed largely of keratinocytes
- Renewed continually approx. every 4 weeks in healthy adults
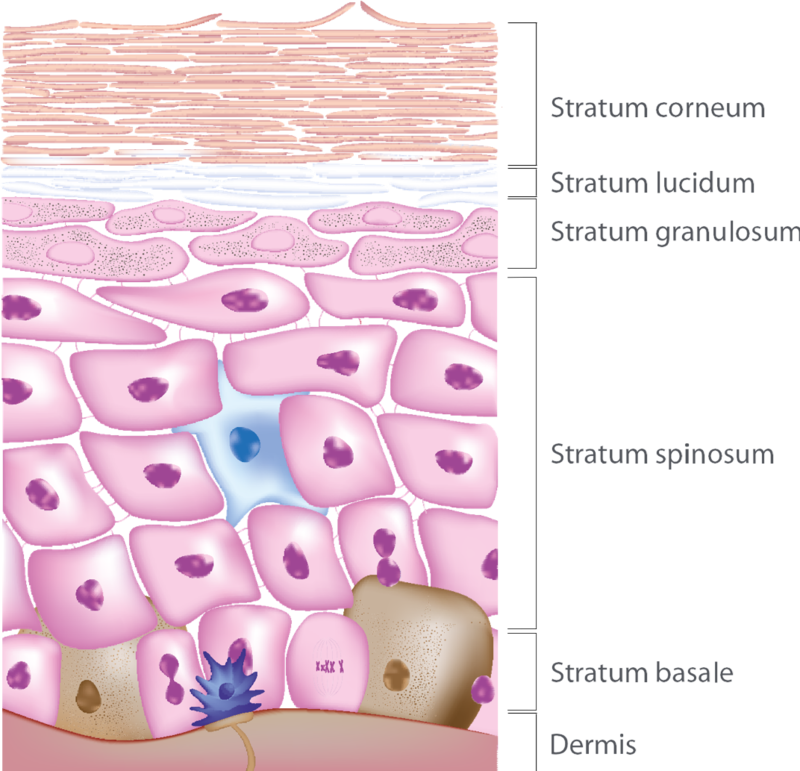
The body’s outermost protective layer is the multi-layered epidermis. Physiologically speaking, this squamous epithelium is comprised of keratinized cells moving slowly towards the surface which consists of up to 95 % of these cornified cells, called keratinocytes. The epidermis must constantly renew itself in order to fulfill its function as a barrier. This renewal takes place in a cycle of about 4 weeks.
Unlike many other body cells, skin cells can renew themselves through cell division throughout our entire lives. The division takes place in the basal layer (Stratum basale), the innermost layer of the epidermis, which is connected to the dermis through the dermal papillae - nipple like extensions - that supply oxygen and nourishment. The epidermis itself has no blood vessels. In the epidermis, there are several other cell types such as melanocytes that synthesize the pigment melanin when stimulated by UV light. The skin’s immune system includes Langerhans cells which also play a role in the development of skin allergies. The epidermis also contains special mechanoreceptors, Merkel cells, which are responsible for the sense of touch.
Anatomically, the epidermis essentially consists of four layers of keratinocytes at different stages of differentiation. Between the basal cell layer and the Stratum corneum (horny layer) there are the transitional layers Stratum spinosum and Stratum granulosum (granular cell layer). The Stratum lucidum (clear layer) outside of the Stratum granulosum is only present in the palms and soles of the feet. Through the formation of new cells, overlying cells are continuously pushed upwards. The cells change as they move upwards, flattening and becoming larger. The cells keratinize and dehydrate slowly and turn into corneocytes which form which form the Stratum corneum (outermost layer). At its surface they are then shed as dead skin cells (desquamation). Our skin sheds up to 14 g of these cells per day.
The Stratum corneum or horny layer of the epidermis is the outermost barrier layer of the skin.
A disturbance in this area can lead to problematic skin conditions and skin diseases.
CUTANEOUS APPENDAGES
- Specialized skin structures that arise from the epithelial cells of the epidermis anchored in the dermis
- Functionally independent of the skin
Subdivided into:
- Cutaneous glands
- (sebaceous glands, sweat glands and scent glands)
- Nails
- Hair
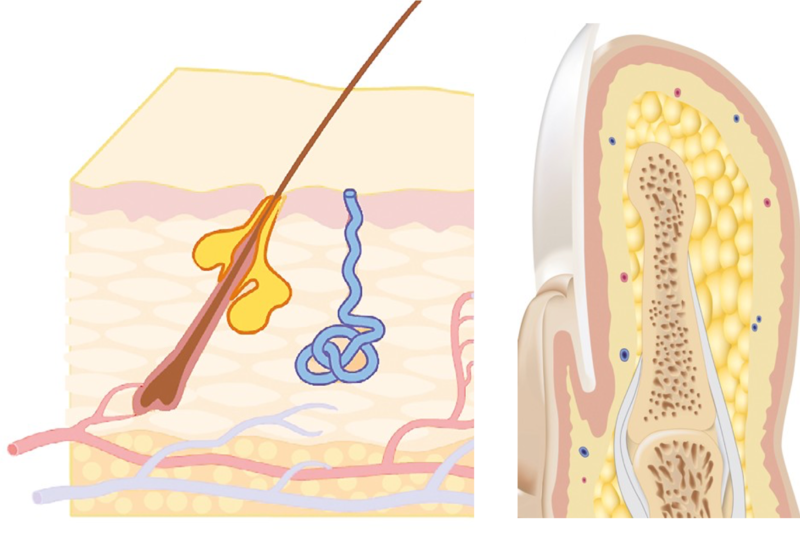
Among the skin’s appendages are nails, hair and skin glands (glandulae cutis). They develop from invaginations of the epidermis into the dermis.
Skin Glands
The skin’s glands include the sweat, scent, sebaceous and mammary glands. Their activity is controlled by hormones. Sebaceous glands are almost always linked to a hair follicle which releases a lipid-containing secretion (sebum) to the skin surface through its funnel-shaped opening. They are holocrine glands in which the entire gland cell is converted into secretion. The largest sebum glands are found on the face. The number of glands varies with location. Many are situated on the forehead, nose, chin, chest, upper back and upper arms, while the forearms, lower legs, palms and soles contain less. The sweat glands are among the eccrine glands in which the secretions pass through the cell membrane. Along with aqueous sweat, electrolytes, weak acids (metabolic degradation by-products) and urea are released onto the skin’s surface.
Both sweat and sebum are important parts of the hydrolipid film as well as the acid mantle. The activity of the two types of glands is vital for the skin’s condition.
Nails
The nails are horn-like plates which rest on the nail bed at the tips of the fingers and toes. They are about 0.5mm thick and can be free at the front edge of the nail body. They grow in a skin pocket (the proximal nail fold).
Depending on the circulation and metabolism, renewal of the nail takes 6 - 24 months. Diseased nails can be signs of systemic disease, deficiencies or fungal infections.
THE STRUCTURE OF HAIR
Structure and Composition of Hair
- Keratinous strands that protrude from the follicles
- Formation in the hair follicle, a sack-like depression in the dermis
- Consisting to approx. 90 % of keratin
- Optimal structural stability and protection at a pH of 5.5
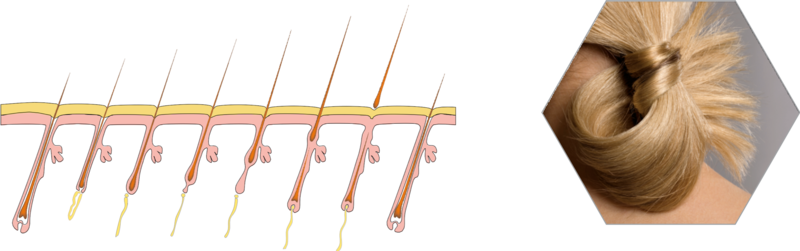
The term hair denotes two structures: the hair shaft extending from the skin and the hair root. The root is at the end of the hair bulb and together with the underlying dermal papilla, is responsible for the hair‘s nourishment and growth. A sheath of tissue surrounds the entire hair follicle and comprises the hair follicle unit.
A strand of hair consists of three layers:
The marrow (medulla), a loose layer of cells inside the hair.
The cortex, which forms the main part of the hair. It consists of fine keratin bundles and gives the hair stability.
The outer cuticle layer (cuticle), which coats the cortex. It consists of flat, thin cells laid out like shingles. This protects the hair.
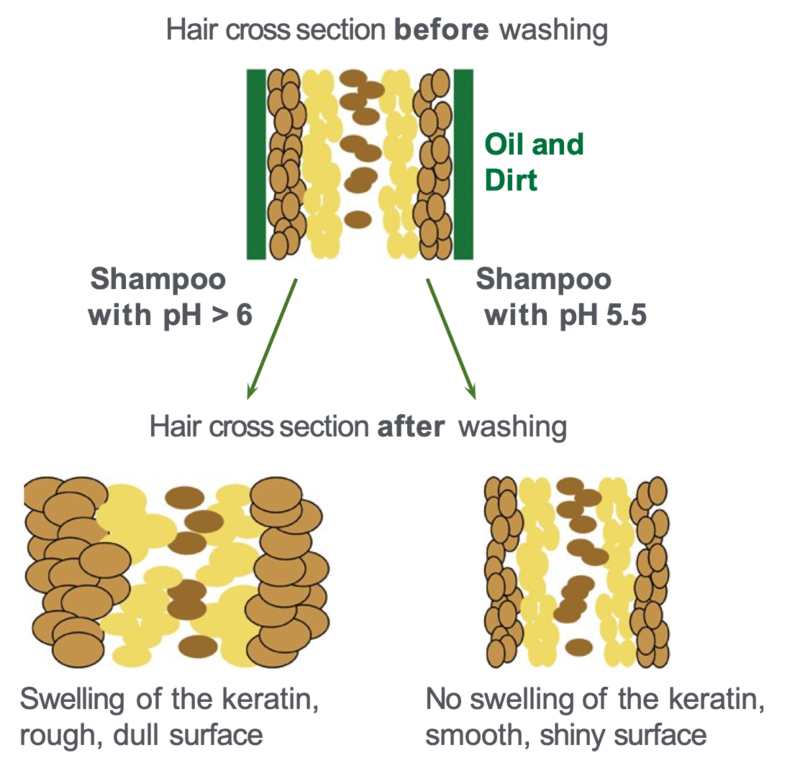
Hair is made up to approx. 90 % of keratin, a fibrous protein molecule that turns inwards in a spiral. The structure of keratin is influenced by the pH value. When washing or applying hair treatments the effects are clearly visible.
Keratin is composed of various amino acids that induce positive and negative electrical charges in the molecule. At the so-called isoelectric point the charges are balanced and the molecule is outwardly neutral. Here the stability of the keratin is greatest. The isoelectric point of keratin is at a pH of 5.5.
Higher pH values swell the hair. Although this increases the hair’s volume, it simultaneously weakens the chemical and mechanical resistance of the hair and promotes dehydration. In addition, the surface (the cuticle) becomes irregular, which reduces light reflection so that the gloss is lost. Also, the resistance increases during combing and with it the risk of damage from split ends and breakage increases.
HAIR AND SCALP
- Cyclic growth
- Cycles last up to 8 years
A healthy scalp with a strong supply of blood is the basis of healthy hair!
The hair doesn‘t grow constantly but each hair follicle undergoes repeated growth cycles, which consist of three phases. During the growing phase (anagen), a hair matrix producing keratin is created in the root sheath and forms the hair shaft. At the same time the pigmentation takes place through melanin. The duration of this phase is between 2 and 8 years for the hair on the head. About 80 - 90 % of the hair is in this phase.
In a transitional phase (catagen), a degeneration of the root and the hair matrix takes place which leads to the death of the producing cells. A maximum of 1 % of the hair follicles is in this phase which lasts 2 to 3 weeks.
The hair then becomes loose because it is no longer firmly anchored in the deeper skin layers. This period of approximately 3 months is called a rest phase (telogen). Towards the end of this phase new hair follicles are developed which then start into a new anagen phase. Hair growth is asynchronous so that the individual follicles are located in different sub-phases and natural hair loss is almost constant. Between 60 and 100 hairs per day can be shed.
The scalp has a significant influence on the growth of hair. When the scalp is healthy and well supplied with blood, the hair papillae are well nourished and hair grows strongly at a maximum rate. The use of a mild, soap-free shampoo with pH 5.5 which does not dry out the scalp and protects the natural acid mantle also protects the hair and its structure. This is important for healthy and beautiful hair.
THE SKIN MICROBIOME
- The skin surface is colonized by micro-organisms
- The skin microbiome is important for skin health and skin diseaes are often associated with or caused by a microbial imbalance
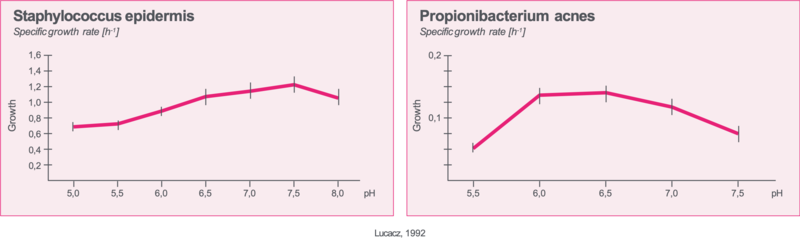
- pH 5.5 favours the skin‘s healthy microbiome balance, supporting the protective effectof species like Staphylococcus epidermidis, suppressing Propionibacterium acnes and Staphylococcus aureus
A mapping of the complete skin microbiome with novel methods provides additional insights in the complexity of interactions. Future research will lead to a better understanding of how skin cleansing and care affects the
microbiome balance and through it the skin’s health. Based on decades of research pH 5.5 is not only a stabilizing factor for the skin’s chemical and physical, but also for the microbial barrier function. Similar to the role of a healthy nutrition for the gut microbiome, skin cleansing and care with a pH of 5.5 supports the protective functions of a balanced skin microbiome.
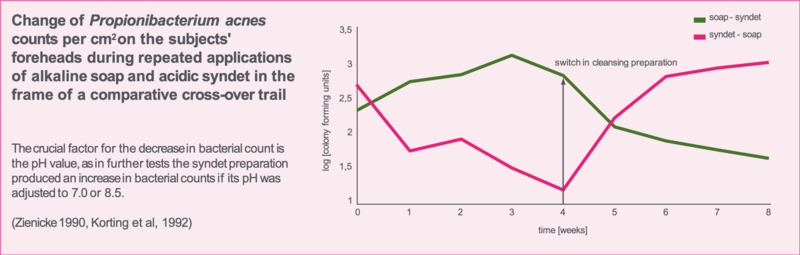
The whole skin surface is populated by specially adjusted micro-organisms. Research from 80 years ago already revealed beneficial effect of apathogenic microbes on the skin’s health and suggested a defensive function against pathogenic species. The skin surface pH is a regulatory factor for the healthy microbial balance as proven in vitro by cultivation of various bacterial species at pH 5.5, 7.0 and 8.0, respectively and also in vivo for Propionibacterium
acnes. Like Staphylococcus aureus this species is associated with a skin disease and it proliferates in neutral or alkaline milieus caused, e.g., by using soap for skin cleansing. Staphylococcus epidermidis, a non pathogenic germ, is by contrast growing well at pH 5.5. As a dominant bacterial species on human skin it keeps the noxious intruders in check and also probably positively affects the skin’s immune responses to infections.
THE SKIN‘S STRUCTURE
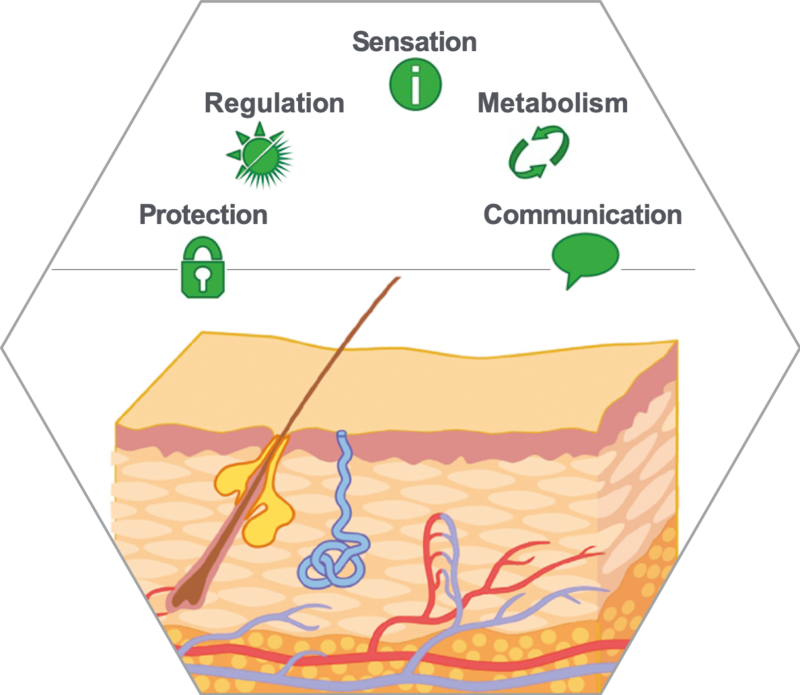
Healthy skin can and must fulfill many different functions:
Protection: The intact Stratum corneum protects against excessive dehydration.
A certain degree of evaporation through the skin is normal; this is called transepidermal water loss (TEWL). The skin also protects against the entry of exogenous substances
(in whole or in part). This phenomenon is known as a penetration barrier.
The skin can return to its original shape after being stretched. In addition, subcutaneous adipose tissue has a padding effect which protects the internal organs from external physical trauma (mechanical protection).
A buffering capacity allows skin to recover its physiological pH value after contact with alkaline substances
(chemical protection). Protection against UV-light is achieved through mechanisms such as tanning or the thickening of the Stratum corneum as a physical protection.
Regulation: Changes in blood flow and evaporative cooling can control the body temperature.
Sensation: Mechanoreceptors (touch), temperature and pain receptors provide sensory information to the brain. At the same they can trigger protective reflexes that protect the skin even more quickly.
Metabolism: The excretion of degradation products, for instance uric acid and amino acids, can be effected through the skin. Also the formation of Pro-Vitamin D takes place in the skin.
Communication: The appearance of a human being is determined by the individual skin type and skin appearance. Mechanisms such as blushing or becoming pale also show on the skin's surface.
THE BARRIER FUNCTION
Hydrolipid Film
- An emulsion made up of lipids and water with hydrophilic substances on the epidermis
- Keeps the skin supple
- Provides protection against harmful microorganisms
- Composed of sweat, corneocyte debris, sebaceous lipids, amino acids, lactic acid and natural moisturizers
The hydrolipid film is part of the skin’s barrier and covers the entire skin’s surface as an emulsion. Depending on its composition, it is either a W/O (water-in-oil) or O/W (Oil-in-water) emulsion.
Composition and quantity may vary depending on genetic predisposition, body part, external factors such as season or climate and internal influences such as illness, stress or age. This determines the skin condition to a large part.
The aqueous part of the emulsion is formed from sweat and transepidermal water. The sweat also contains hydrophilic substances such as electrolytes (e.g. sodium ions, chloride), various organic acids from endogenous metabolic processes (e.g. lactic acid, acetic acid or uric acid) or urea from the epidermis.
The lipophilic part of the hydrolipid film mainly comes from the sebaceous glands. These are triglycerides, wax esters and squalene. Also included are weak organic acids which, together with the water-soluble acids and corresponding salts, form a buffer system that stabilizes the pH environment in the hydrolipid film to values of between 4.5 and 6.
Desquamated corneocytes are also found in the hydrolipid film.
An intact hydrolipid film is crucial for the skin’s health. Insufficient production of sebum and/or sweat leads to drier skin that usually feels taut, is rough and scaly and often itches. In addition, the barrier function is no longer fully functional so that irritants can easily penetrate the skin (which can lead to infections or eczema). An overproduction of sebum, though, leads to seborrhea and can manifest itself in skin blemishes or skin disorders such as acne and seborrhoeic dermatitis.
The Acid Mantle
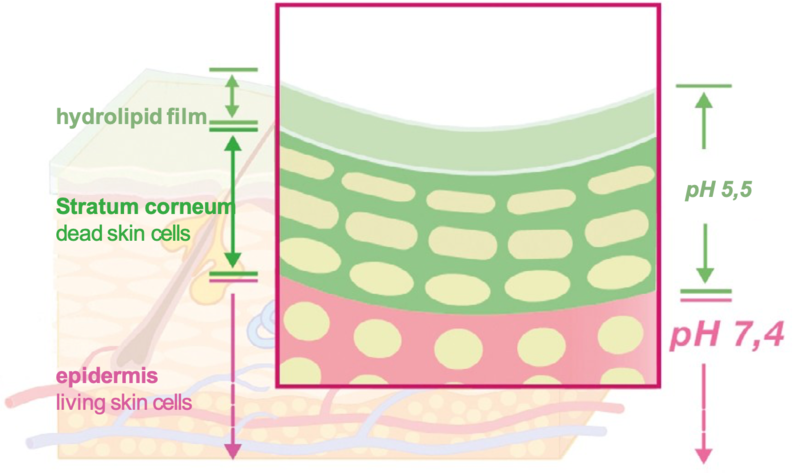
- The hydrolipid film and the Stratum corneum are mildly acidic
- Physiological environment for a healthy skin microbiome
- Control of the skin’s alkali neutralization capacity
- Activation of enzymes (e.g. acid hydrolases for ceramides - an important component of the epidermal barrier)
The surface of healthy skin in humans from infancy to adulthood to old age has a slightly acidic pH. This is called the acid mantle of the skin. Responsible for the pH-value are weak acids from sweat, sebum (see previous page), cornification (the degradation of keratin to glutamic acid results in pyrrolidine carboxylic acid), the transformation of epidermal lipids to Stratum corneum lipids, the activity of Na+ /H+ antiporters in the Stratum granulosum and acidic metabolic by-products of microorganisms belonging to the skin flora.
Depending on the part of the body, pH values lie in the range of 4.5 and 6.0. The average pH value of the skin is 5.5. Different values may be present in the armpits, anal folds or the genital area. These areas have a pH of up
to 6.5. The term acid mantle refers to various protective mechanisms. The pH value of 5.5 creates a beneficial physiological environment for a healthy skin microbiome and counteracts dominance of certain species like Staphylococcus aureus or Pityrosporum ovale which is associated with skin diseases. pH-values of 6 or more favor pathogenic microorganisms whose growth is at an optimum in the pH neutral range.
Also, the buffering capacity (the stabilization of the pH value) against pH changes such as those caused by soaps is controlled by the acid mantle. In healthy adults, it takes up to three hours after washing with a classic soap to restore the initial pH value. The longer this process takes, the greater the risk of skin damage, especially in children or older people.
The acidic pH also plays a role in the formation and structure of the epidermal lipids in the Stratum corneum and is important for the function of the permeability barrier in the epidermis. For the formation of epidermal lipids, enzymes such as b-glucosylcerebrosidase, acidic sphingomyelinase and phospholipase A2 are required which catalyse reactions yielding acidic products, thus generating an acidic pH.
The Epidermal Barrier
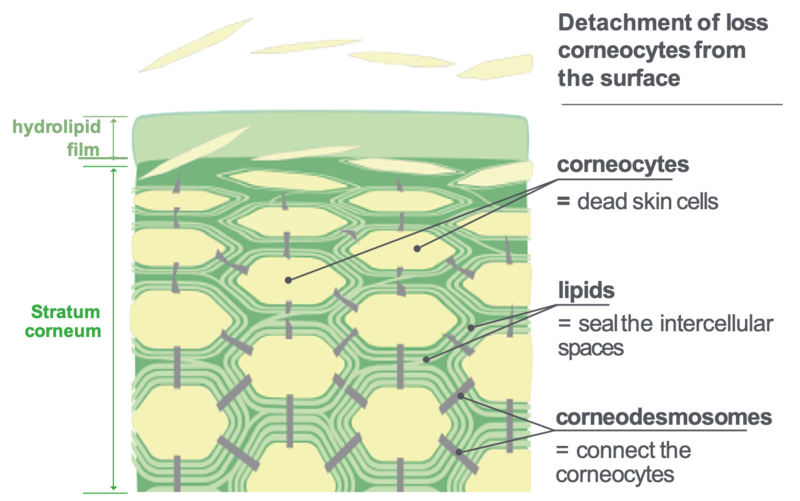
- Efficient permeability barrier
- Consists of corneocytes (final differentiation stage of keratinocytes in the Stratum corneum) an epidermal lipids
- Stratum corneum cohesion and integrity mediated by filaggin, involucrin and corneodesmosomes
- Lipophilic structures consisting of bilayer lipid membranes with ceramides, chlesterol and free fatty acids
- Contains natural moisturizing factors (NMF)
Specific proteins provide stability to the Stratum corneum and the epidermal barrier. Filaggrin aggregates the keratin filaments in the interior of the corneocytes and connects them with the so-called cornified envelope of which Involucrin and Loricrin are main constituents. Individual corneocytes are linked by corneodesmosomes consisting of proteins, too. This ensures the structural integrity of the “bricks” and provides a solid scaffold for the extracelluar lipids - the mortar.
In the uppermost layer of the epidermis, the Stratum granulosum, the transformation of the keratinocyte to a corneocyte starts with the development of the cornified envelope and keratin crosslinking by filaggrin. Furthermore, the junction proteins Desmoglein 1 and Desmocollin 1 between the keratinocytes are enzymatically immobilized and Corneodesmosin is joined to the aggregates. Transglutaminase is a key enzyme in the transition processes.
LIVING WITH OUR SKIN
A state of change …

- Skin type (light - dark) genetically predetermined
- Our skin is exposed to internal and external influences a life long
- The skin condition changes
The skin condition is the result of the state of the physiological structures and functions of the superficial skin layers as influenced by the various protective mechanisms: the hydrolipid film, acid mantle and epidermal barrier.
The skin condition changes, depending on age, climate or other internal (intrinsic) or external (extrinsic) factors. Genetic factors determine a basic skin type that can be described as a normal, dry or oily. Genetic factors also affect pigmentation. Hormonal regulation mechanisms or the number of receptors to which hormones can attach themselves are also genetically determined. The hormone status plays a role in, for instance, the formation of oily or dry skin conditions and the development of acne.
The skin condition is determined by the amount and composition of the hydrolipid film and serves as a basis for assessing appropriate cleansing and care. We can distinguish three basic skin conditions:
Normal
Oily (more hydrolipid emulsion)
Dry (less hydrolipid emulsion, weak barrier function)
Babies and young children have a weak hydrolipid film and barrier function so that the skin is rather dry. This state changes only slightly until the onset of puberty. Then hormones influence the production of sebum and sweat and the skin becomes oily in the majority of cases. Male adolescents are usually more affected by this than females.
With the progression of biological ageing, production is lower, the regeneration of skin cells slows and the skin becomes drier once again.
In the spectrum of individual habits and behavior …

- Cleansing and care
- Diet
- Sleep
- Occupational factors
- Mental stress
- Alcohol, tobacco, medication
- Exposure to irritants and air pollution
- Leisure and athletic activities
Our individual lifestyle contributes significantly to the appearance and health of our skin. A number of factors influenced by us determine the condition of the skin - not only the genetic and environmental factors.
Cleansing and care of the skin have a major impact. Unsuitable products can dry out the skin or lead to reactions such as the formation of blackheads and pimples. Conversely, individually tailored cleansing and care of healthy skin increases the resistance to external influences.
It has long been known that a Vitamin deficiency can also affect the skin. For example, a deficiency of Vitamin B2 (riboflavin) can lead to angular cheilitis or seborrhoeic dermatitis. Similar symptoms and sores in the mouth can be caused by a deficiency of pyridoxine (Vitamin B6). Dehydration becomes visible in the skin as well. The skin becomes drier and loses its elasticity.
Sleep can rejuvenate the skin as cell division takes place faster than during the day. If the sleep phases are too short, the skin looks pale and is less resistant. Stress can have a similar effect: the skin may react with pimples and become sensitive to external influences.
Stimulants such as alcohol or nicotine alter the skin’s blood flow and thus influence the nourishment of the cells and their growth.
Irritating or allergenic substances such as those used in a work environment or inadequate cleansing and care products can reduce the barrier function of the skin or trigger inflammation. Long-term exposure to air pollution accelerates ageing processes in the skin. Soaps destroy the acid mantle. These and other factors strain and damage the skin.
Relaxation and regular exercise are good for the skin as blood circulation is promoted. It should be noted, however, that exercise stresses the skin so that individually adjusted skin care is a must.
In the spectrum of global environmental factors …

- Climactic zones
- Effects of the sun
- Influences through ozone
- Influences through pollution
- Oxidative stress
Environmental factors influence our skin significantly. Warm, humid climates enhance the production of sweat.
In this climate, the hydrolipid film is well developed and skin accustomed to this climate is more resilient. In colder climates, the skin becomes drier and more sensitive. Below a temperature of 8 degrees Celsius, sebum can no longer spread across the skin because its viscosity becomes too high and thus its fluidity is insufficient. With lower humidity, the barrier function is weakened. The effect is clearly visible through changes to the skin in the summer and the winter or when traveling through different climactic zones. Skin care should be adjusted to the climactic conditions.
The sun also has a great influence on the skin. We have natural protection against UV - rays which is adjusted to our regional conditions and prevents damage to the skin. UV radiation is also filtered by the ozone layer in the
atmosphere. Due to the destruction of the ozone layer, there are holes over the poles which allow more UV radiation to reach the ground. This can cause skin damage (see the following pages). Areas strongly affected by this include Australia, Canada, Scandinavia and parts of Central Europe. Individual, mild skin care and the appropriate sun protection is important.
The global problem of pollution is caused by automobile exhaust particulate matter emissions from diesel engines, industrial emissions or water pollutants. The skin is exposed to irritants more often and becomes more sensitive.
The particulate pollutants may lead to a blockage of the pores which then leads to the formation of blackheads or pimples and promotes the development of pigment spots and wrinkles, most probably mediated by enhancing free radical formation in the skin.
Skin damage can also result from the influence of alcohol, nutrition, diseases, the work environment or increased physical activity. The stress caused by the highly reactive oxygen species is called „oxidative stress“. Lipids which have one or more double bonds such as some of the barrier lipids of the Stratum corneum are negatively affected. Free radicals are also responsible for the activation of enzymes and the degradation of collagen and elastin fibers which results in accelerated skin ageing.
In the spectrum of the Sun …
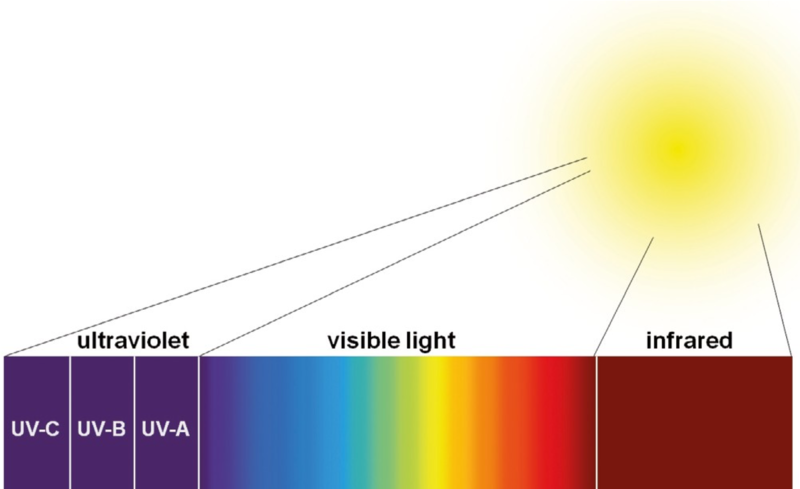
The sun produces multiple different types of radiation. The shortest wavelengths are almost completely filtered by the ozone layer in the atmosphere.
The sun’s spectrum includes the following types of radiation as a function of wavelength:
Ultraviolet (UV) light (10 %)
Visible light (50 %)
Infrared (thermal) radiation (40 %)
The ultraviolet light has the strongest effect on the skin. UV light is divided into three categories according to the wavelengths: UV-A, UV-B and UV-C. UV-A and UV-B have the greatest influence on the skin.
UV-A radiation (wavelengths 320 - 400 nm) can penetrate into the dermis (> 50 %). It penetrates window glass and is responsible for rapid tanning (immediate pigmentation), premature skin ageing due to elastosis, phototoxic and photoallergic reactions. It also triggers polymorphic light eruption, immune suppression and the development of skin cancer.
UV-B radiation (280 - 320nm) acts on the basal cell layer where it is responsible for the permanent tan. An excess of UV-B radiation causes sunburn (inflammation) and changes in DNA. It also stimulates Vitamin D synthesis from cholesterol and other metabolic processes.
UV-C radiation (200 - 280nm) is the most energetic but the rays are filtered by the ozone layer. In areas affected by the ozone holes, they can reach the earth but only to penetrate into the Stratum corneum. They are strongly erythemogenous and possibly carcinogenic.
Infrared rays are heat rays that are able to penetrate into the subcutaneous tissue. Prolonged exposure triggers heat sensation, perspiration, pre-mature ageing and dehydration of the skin.
Influence of the Sun …

Positive effects
- Well being
- Synthesis of Vitamin D
- Stimulation of metabolic processes
Negative effects of overexposure
- Sun burn
- Premature skin ageing
- Skin diseases
- Skin alterations
Small doses of solar radiation has a positive effect on our body. Our immune system is stimulated, our mood improves and metabolic and circulatory processes are stimulated. One of the most important processes is the stimulation of the synthesis of Vitamin D in the epidermis. The energy of UV-B radiation is essential in forming Vitamin D3, Cholecalciferol, from the precursor 7-Dehydrocholesterol (which is present in the skin naturally).
The skin has several protective mechanisms that are triggered by UV exposure and prevent damage within limited exposure:
- Tanning (pigmentation of the skin and protection of the cell nuclei)
- Hyperkeratosis (thickening of the epidermis through ultraviolet rays)
- Urocanic acid (UV-absorbing amino acid in sweat)
- Repair mechanisms through enzymes that repair UV-damaged cells
- Exposure to UV radiation exceeding the skin’s self-protective mechanisms (minimal erythema dose, MED) leads to a solar erythema or sunburn. This is an inflammation caused by an overdose of UV-B rays.
- Amongst the consequences of chronic light damage are premature skin ageing, precancerous lesions such as actinic keratoses and skin cancers (basal cell carcinoma, squamous cell carcinoma and melanoma).
- Premature skin ageing through enzymes (matrix metalloproteinases) is induced by UV-A radiation and accelerates the degradation of collagen fibers. This leads to a loss of skin elasticity and wrinkles.
- Precancerous lesions and cancer are the results of malign cell proliferation due to the damage to their DNA.
- UV-A radiation can also cause pathogenic reactions of the immune system which are known as polymorphic light eruption. These include sun allergy and Mallorca acne.
Athletics

Positive effects through regular physical exercise
- Improved circulation
- Improved regenerative capacity
- Heavy perspiration
- Frequent showers
- Chlorinated pool water
- Mild cleansing and care with pH 5.5 products for the skin prevents irritation
Regular exercise not only helps the circulatory and musculoskeletal systems, but also our skin. Circulation improves so that the skin is supplied with more oxygen and nutrients. Excretion of metabolic degradation products is facilitated. The regeneration of skin cells is improved and the skin looks brighter and smoother.
However, exercise also places a burden on the skin. Due to the increased body temperature, sweating is increased in order to cool the body. The moisture evaporates on the skin and cools - but also leads to enhanced dehydration of the skin.
Showers should be taken shortly after exercise and at about body temperature so that the acid mantle and the barrier function are not disturbed excessively. A study by Professor Martina Kerscher showed that moisture balance, barrier function and acid mantle of the skin are stressed during exercise and athletics but can be stabilized by a soap-free shower at the physiological pH 5.5. A mild cleanser with a pH of 5.5 should be used to support the
natural defense of the skin against infections with fungi or bacteria. Depending on the skin condition, products with moisturizing or emollient additives can also be recommended.
Chlorinated water in swimming pools leaves the skin even more stressed because, in addition to the drying effects of water, chlorine irritates the skin. It is important to thoroughly rinse off the chlorine with a mild skin cleansing agent at a pH of 5.5. Afterwards, the skin should be nourished with a product that is also adjusted to the pH balance of 5.5 and provides lasting moisture and lipids.
Requirements for cleansing and care:

- Individually tailored to the skin
- Regular use
- Cleansing must be gentle
- Adjusted to pH of healthy skin (pH 5.5)
- No drying, no irritation
- Care must be effective
- High-quality, tested ingredients
- Adjusted to pH of healthy skin (pH 5.5)
Supporting and restoring the acid mantle and barrier function
Regardless of age and skin condition, the skin must be regularly cleansed and cared for. Skin cleansing and care should take place with mild, gentle, effective ingredients that do not damage the skin’s barrier function and the physiological acid mantle.
Proper washing keeps the skin healthy. Incorrect cleansing products can dehydrate and irritate the skin. Gentle cleansing with a mild syndet that matches the skin’s natural pH of 5.5 is important regardless of skin condition. By adjusting the sebamed products at these pH values, the natural acid mantle is preserved. The
protective functions of the skin remain intact or can be restored with problematic skin conditions. The mild syndets do not cause irritation and the skin's healthy micro-flora is not affected. By stabilizing and regulating the natural protective mechanisms, effective protection against infection (bacteria, fungi) is attained.
sebamed cleansing products are suitable for the entire body and the face. Excluded are products with urea for extreme dry skin as well as products for the genital area.
Through the careful cleansing, the skin is optimally prepared for subsequent care. The skin care products sustain the natural protection of the skin or compensate for deficiencies and the effects of care is sustainable.
sebamed uses only high quality, tested ingredients. A superior tolerance and efficacy of skin care with a pH of
5.5 has been demonstrated in a multitude of clinical studies.
In one study, the importance of pH for the protective and regenerative properties of a hydrophilc emulsion was investigated. Only the emulsion with pH 5.5 leads to a stabilizing effect on the epidermal barrier function (see Study: Gehring W.: The Importance of pH for the Vehicle Effect of a Hydrophilic Emulsion and its Consequences for the Protective and Regenerative Properties, Akt Dermatol 2016; 42: 349 - 352).
